Hidden Enemy: Why TB Remains One of the World’s Deadliest Diseases
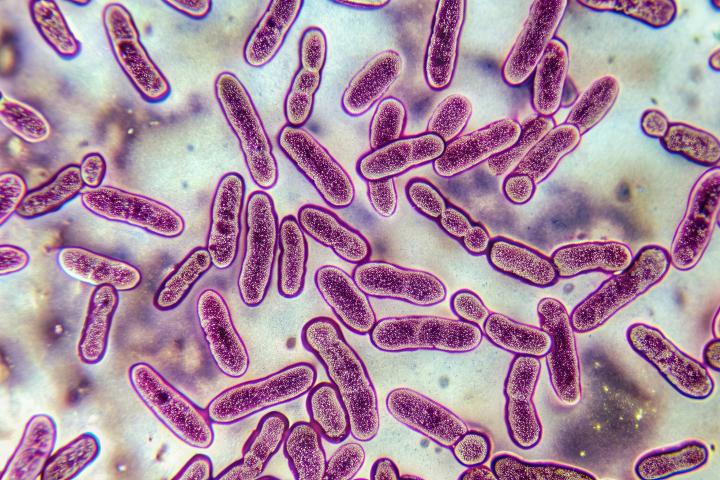
Gram-stained image of Mycobacterium tuberculosis bacteria colonies on a histology slide, with distinct morphology and growth patterns (Photo: Supplied)
For more than a century, we’ve known that Mycobacterium tuberculosis (Mtb), the bacterium that causes tuberculosis (TB), is a master survivor. But, only now, are scientists beginning to fully grasp just how adaptable and elusive it really is.
An exciting new review in Nature Reviews Microbiology — led by UCT’s Institute of Infectious Disease and Molecular Medicine (IDM), Professor Digby Warner and Professor Emerita Valerie Mizrahi, together with their collaborators from the Ragon Institute (USA) and the Francis Crick Institute (UK) — details recent insights into the age-old interaction between Mtb and humans. The picture they present challenges us to see Mtb as it really is: a shape-shifter, an opportunist, and a global threat that continues to confound simplistic assumptions about its capabilities.
The Silent Spread
We often think of TB as a coughing, feverish illness that affects only the lungs. The reality is much more complicated: infection with Mtb doesn’t always make people sick. In fact, most people who are infected never show symptoms, yet may still be able to pass it on — an unsettling concept we learnt to accept with SARS-CoV-2/COVID-19.
You may be carrying Mtb for years without knowing, with the bacteria remaining alive and undetected in the body in hiding places that include bone, brain, and lymph nodes. Mtb has the ability to wait, sometimes for decades, until the immune system is distracted or weakened — and then it reactivates. In high-burden settings such as South Africa, though, continual exposure to airborne Mtb organisms means that re-infection, rather than reactivation, is likely to be the dominant driver of new TB disease.
How Mtb Outsmarts the Body
Unlike other bacteria, Mtb doesn’t seem to be in a rush. Having evolved with humans for thousands of years, the bacterium has learned to do three things exceptionally well:
- Hide: Mtb slips inside human cells – including the very immune cells designed to kill it –and uses them as a safe haven.
- Adapt: Mtb changes how it produces energy according to its environment, slowing down in tough conditions like low oxygen or limited availability of essential nutrients.
- Survive: Mtb builds a waxy, armour-like outer shell that makes it hard to kill — even with antibiotics.
This slow and steady strategy is part of what makes Mtb so dangerous. Even when our bodies mount a defence — forming immune cell clusters called granulomas to trap the bacteria — Mtb often finds a way to escape, especially in the lungs where it can gain access to the airways to be expelled into the air and infect someone else.
New Tools, New Thinking
What this review makes clear is that, to outsmart Mtb, we need to change how we study it.
Instead of using only laboratory models or animals, researchers are turning to human tissue samples, spatial and single-cell analyses, and advanced imaging to observe how Mtb behaves inside real people. This shift in focus from petri dish to patient could unlock answers we’ve missed for decades.
As Professors Warner and Mizrahi and their co-authors argue, TB isn't just about the bacteria or the person infected — it’s about the whole system: Mtb, the lungs, the immune system, even the air we breathe.
Hope on the Horizon
Despite the complexity, there is hope. Promising new vaccines and shorter, smarter treatments are on the way. Scientists are also exploring how to boost the body’s own defences using what’s called “host-directed therapies” to help the immune system respond more effectively.
But, to win this battle, we must first understand the adversary, not just in the lab, but in its natural host: us.
Read the full article on Springer Nature:
Mycobacterium tuberculosis biology, pathogenicity and interaction with the host.
